Lasers could help doctors diagnose cancer earlier and more reliably, and in a less invasive way, says Tufts biomedical engineer
Identifying suspicious growths like these is just the beginning of a long road toward diagnosis and eventual treatment. At the moment, the only way to verify if cells are diseased is to perform a biopsy, a minor surgery in which doctors and pathologists remove a small piece of tissue, and inspect thin slices of it under the microscope.
It’s a painstaking process, and according to Irene Georgakoudi, it’s an imperfect one. Since the suspicious lesions are identified visually, dangerous cancers can sometimes be missed—and even if they aren’t, an accurate diagnosis often comes too late.
“By the time things become visible enough to raise suspicion, a tumor has likely already invaded surrounding tissue, and it becomes very difficult to treat,” she says. If doctors were better able to identify cancerous cells before they spread, she adds, patients would have a much better chance of being cured.
So Georgakoudi, an associate professor of biomedical engineering at Tufts School of Engineering, is researching methods to diagnose cancer at a cellular level, well before it grows into a visible lesion or tumor. In a process she calls an “optical biopsy,” she eschews needles and knives, and turns to much more exotic tools—finely tuned lasers.
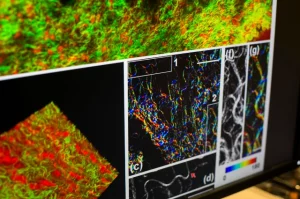
By employing a high-powered pulse of light, she says, her team can take a “snapshot” of the complex chemical reactions at work inside a cell, revealing abnormal activity before any tumor actually forms. “Cancer is something that happens functionally at the beginning,” she notes. “Before any visual changes appear in a cell, there are a bunch of biochemical and fine organizational changes that pathologists can’t currently detect.”
Molecules to Watch
If doctors were better able to identify cancerous cells before they spread, patients would have a much better chance of being cured. Photo: Kelvin Ma
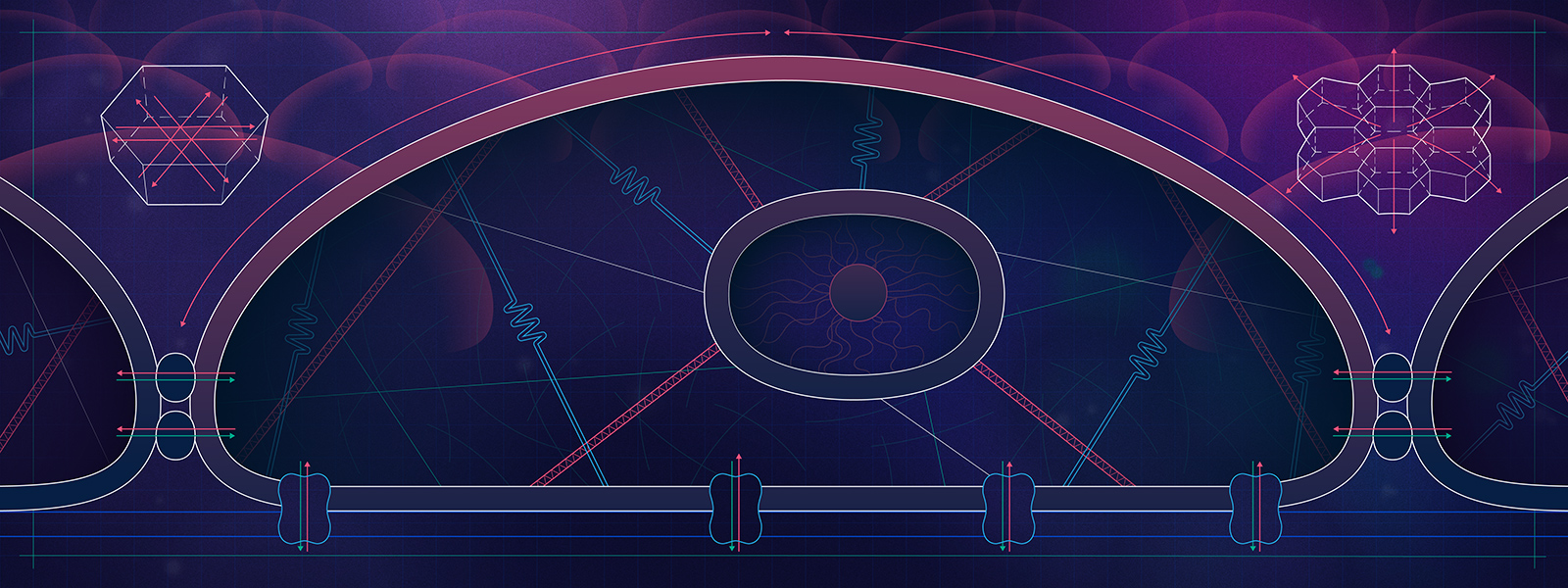
Georgakoudi’s team is able to spot those changes thanks to a unique property shared by two enzymes called nicotinamide adenine dinucleotide (NADH) and flavin adenine dinucleotide (FAD). These molecules play a key role in every cell’s metabolism, the process through which it breaks down sugars to create the energy it needs to survive.
Hit the molecules with the right frequency of laser light, Georgakoudi says, and they’ll momentarily glow, or “fluoresce.” Researchers can measure how bright the glow is, how fast it decays and where it occurs in the cell, picking up clues about how active the enzymes are—and, by extension, how healthy the cell’s metabolism appears to be.
As a cancer grows, its cells’ energy production may speed up, slow down or shift gears entirely, favoring certain types of energy-providing chemical reactions over others. When those changes occur, so do the relative concentrations of NADH and FAD, providing signs that an otherwise normal cell is starting to go off the rails.
Georgakoudi notes that her team doesn’t yet have a clear sense of how NADH and FAD are linked to specific shifts in metabolism. At the moment, they’re using the molecules almost like a car’s “check engine” light—although they don’t point directly to the root problem, they provide a useful sign that something is amiss. Still, that might be enough to identify cancerous tissue, she says. The challenge is to get this information without harming the cell itself.
Triggering the Glow
Coaxing NADH and FAD into a fluorescent state without harming the cells involves hitting them with a huge burst of energy. In order to trigger their telltale glow, the molecules first have to absorb at least two photons (particles of light) almost simultaneously—and they’re not always willing to cooperate.
“The problem is, you need a throw a hell of a lot of photons at them for that to happen,” says Georgakoudi. In other words, the more photons that rain down on the molecules, the more likely it is that two will hit them.
Creating this downpour of photons requires an extraordinarily intense laser—one that can instantaneously pump out several billion watts of power (for comparison, a one-watt green laser is powerful enough to burn human skin, and cause permanent blindness). Normally, using a laser that intense would vaporize the tissue before it would ever cause NADH and FAD to fluoresce.
To get around the issue, Georgakoudi uses lasers that emit light in extremely short, repeated pulses, each one lasting less than a trillionth of a second. “By delivering high-powered pulses that quickly, we keep the average amount of energy that reaches the cells relatively low,” she says. “We’re still delivering enough photons to cause a fluorescent response, but we’re not cooking the tissue in the process.”
Penetration is also an issue, she adds. A focused laser beam reaches less than a millimeter into human tissue, so Georgakoudi is limited to examining cells only on the surface of the skin or organs. Yet this isn’t necessarily a disadvantage, she says. More than 80 percent of cancers initially form in the epithelium, a thin network of cells that form the lining of our skin, mouth, cervix, intestines, stomach and ducts in found in the breast, lung and prostate.
Most of those tissues are accessible to doctors using minimally invasive techniques—the skin, throat and gums are all easily examined, for instance, and even breast ducts and internal organs like the colon and bladder can be reached using special scopes that don’t require doctors to cut into the body. In theory, this would allow “optical biopsies” in areas where most common cancers form.
Ultimately, Georgakoudi wants to expand her technique. She’s currently researching ways to detect cancerous changes not only in the epithelium, but in collagen—the “scaffolding” between cells that gives tissue its structure. That could help determine if a cancer has begun to spread.
She’s also working on ways to spot cancerous cells in the bloodstream, which could offer a real-time assessment of whether chemotherapy or radiation treatment is actually working on a patient. If doctors spot fewer cancer cells floating freely in arteries and veins, she notes, it’s a good sign that the cancer is shrinking.
Georgakoudi is even exploring methods to automate optical biopsies, creating computer software that can instantly identify telltale changes in NADH and FAD fluorescence. If successful, such software might give physicians without specialized training a new tool to reliably diagnose cancer.
Although her techniques aren’t yet ready for clinical use, Georgakoudi is hopeful they could make a dramatic impact on the way cancers are identified—turning a dreaded disease into something that can be managed and treated before it spirals out of control.
“It’s usually not the primary tumor that’s going to kill the patient. It’s the cancers that break off from that tumor and form in the brain or lung or bone,” she says emphatically. “If we could identify the changes that occur early on, before a cancer invades blood vessels and other areas of the body, in most cases we could cure the patient.”
David Levin is an independent science journalist in Boston.